Deep Vein Thrombosis (DVT)
What causes Deep Vein Thrombosis? (DVT)
Deep Vein Thrombosis (DVT) causes can be both genetic and behavioral. A family history of parents or siblings suffering from blood clots can increase your own DVT risk. An undiagnosed clotting disorder can put you at risk of DVT, as well. Behavior-related causes of DVT include smoking and obesity.
Other contributing for DVT include but are not limited to:
- Surgery or traumatic injury
- Cancers and their treatments, both of which may adversely affect the blood’s ability to clot
- Other serious illness, such as congestive heart failure, heart attack, stroke or sepsis
- Varicose veins
- Pregnancy
- Contraceptives/ Estrogen Therapy; this risk especially increases in smokers
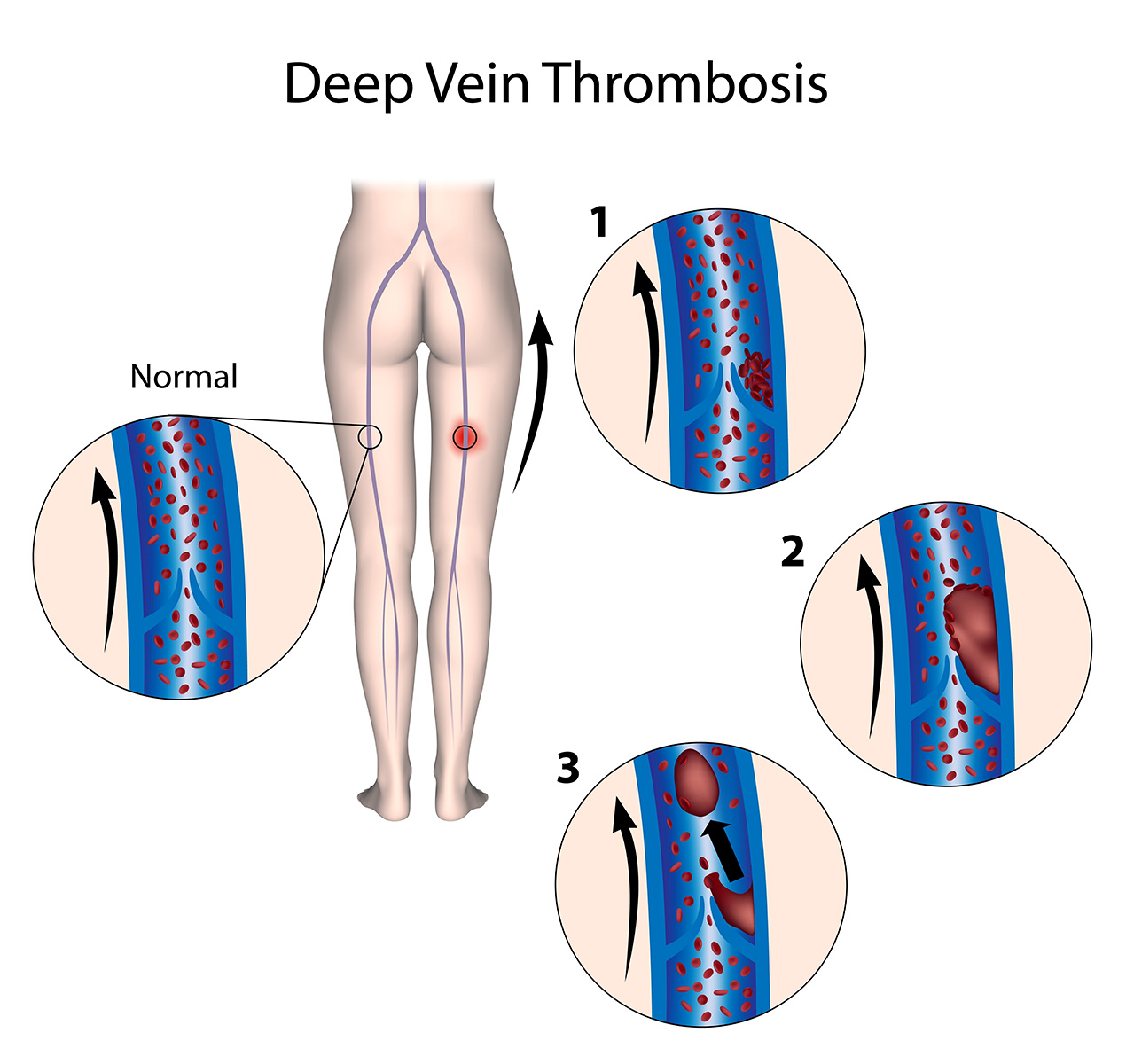
In terms of events that may “trigger” the condition, specific DVT causes revolve around extended sedentary behavior. When we’re healthy, our muscles help our blood keep moving. But when we’re not moving around, blood tends to pool and clot at the lowest part of the body.
Prolonged bed rest due to illness—and recovery from surgery or trauma—are common causes of DVT. Likewise, sitting on an airplane for six or more hours without moving around is one of the leading causes of Deep Vein Thrombosis. For this reason, DVT is often called “economy class syndrome.”
People who have had an injury to their veins—due to trauma, athletic accidents or surgery—also face higher DVT risk.
There are two main concerns.
If untreated, a piece of a deep-vein blood clot can break loose and travel to the lungs, causing a pulmonary embolism — a potentially life-threatening event that affects approximately 60,000 Americans annually.
The primary treatment to prevent this is anti-coagulation: the administration of blood-thinning medication such as Lovenox, a shot, and Coumadin, a pill. Anti-coagulation generally prevents a clot from moving to the lungs.
However, there is a second reason to be wary of DVT. Even with anti-coagulation, there can be long term consequences, namely something called post-thrombotic syndrome, which results in pain and swelling for the rest of a patient’s life. Our goal here at Vascular and Interventional Physicians in treating DVT is to actively and aggressively prevent post-thrombotic syndrome.
For many decades, the traditional treatment for DVT’s have been “anticoagulants”: A drug that thins the blood and aids in the breakdown of a clot. Some examples of anticoagulants are Lovenox, which is a shot. Coumadin, which is a pill. Another alternative name for Coumadin is Warfarin.
Anticoagulants do not directly treat the clot; however, it prevents a new clot from forming in the hopes that the body will dissolve the clot that’s already there. Anti-coagulation tries to tip the balance in favor of the body dissolving the clot.
The biggest problem with treatment using anti-coagulation alone is that, depending on which studies you look at, despite taking blood thinners, 33-50% of people develop something called “post-thrombotic syndrome” which is lifelong pain and swelling of the legs.
In DVT thrombolysis, a catheter is placed into the vein to remove a stubborn clot. Thrombolysis is a complementary treatment to anticoagulants, so patients using this procedure to address difficult clots will still need to take the blood thinners after the procedure. The goal with DVT Thrombolysis is to get rid of a chronic clot as soon as possible to minimize damage to the important one-way valves, thereby preventing post-thrombotic syndrome.
Thrombolysis is a minimally invasive procedure performed with the patient under sedation. The process of this procedure takes approximately 2 hours.
A small needle is placed into the vein at the back of the knee, and flexible wire is extended into the vein through the clot. Once placed, a specialized catheter is advanced to the site of the clot to dissolve, break apart, and remove the site of Thrombosis.
Our physicians use cutting edge catheters for DVT removal, including the Angiojet, which uses highly pressurized jets of saline to fragment and remove the clot. Trellis is another alternative, which uses a clot-dissolving medicine called TPA to break up the clot and suction it out.

Have questions?
To learn more about how our physicians can help you, contact us directly (602) 200-9339